Objective:
The objective of this study was to examine the characteristics and utilization patterns of palliative care among lymphoma cancer patients using a large-scale representative population-based sample.
Methods:
Retrospective analysis was conducted on hospitalization data from the National Inpatient Sample (NIS) spanning January 2016 to December 2019. The study aimed to investigate the characteristics and disparities associated with the provision of palliative care to deceased lymphoma patients and evaluate its impact on healthcare utilization, specifically discounted hospital charges and length of stay (LOS). Multivariate linear and logistic regression analyses were performed, stratifying the data based on age, race, Charlson comorbidity index, insurance status, median household income, and hospital characteristics. The study population was classified and identified using ICD-10 codes.
Results:
We identified 10,323 deceased lymphoma patients from hospitalization records, among whom 52.9% (n=5,464) received palliative care during their hospital stay.
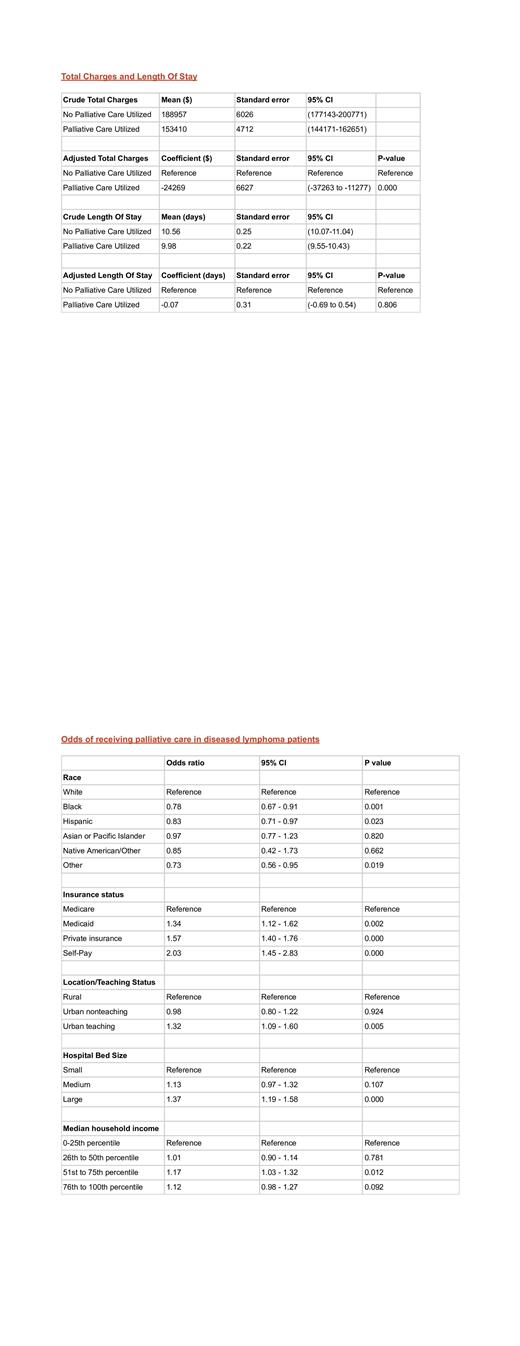
Multivariate linear regression analysis demonstrated that the group receiving palliative care had significantly lower total charges, with a mean decrease of $24,269 (95% CI: $37,263 to $11,277, p < 0.001) compared to the group not receiving palliative care. However, there was no statistically significant difference in the adjusted length of stay between patients who received palliative care and those who did not (coefficient = -0.07 days, 95% CI = -0.69 to 0.54, p = 0.806).
Multivariate logistic regression analysis indicated that patients with Black and Hispanic race had lower odds of receiving palliative care, while those admitted to larger and urban teaching hospitals had higher odds of receiving palliative care. Additionally, patients with Medicare had the lowest probability of receiving palliative care compared to other insurance groups.
Conclusion:
This study provides valuable insights into the utilization patterns and characteristics associated with palliative care among deceased lymphoma patients. The findings demonstrate that receiving palliative care is associated with significantly lower total charges, indicating its potential cost-saving benefits in healthcare utilization. However, no significant difference was observed in the adjusted length of stay between patients who received palliative care and those who did not.
Furthermore, the study highlights disparities in access to palliative care, with Black and Hispanic patients having lower odds of receiving such care. Hospital characteristics, such as size and urban teaching status, were found to influence the likelihood of palliative care utilization. Additionally, patients with Medicare insurance had the lowest probability of receiving palliative care compared to other insurance groups.
These findings underscore the need to address disparities in access to palliative care and ensure equitable provision for all lymphoma patients, irrespective of race or insurance status. Integrating palliative care into the treatment approach for lymphoma patients has the potential to optimize healthcare utilization and improve patient outcomes. Policymakers should consider these findings to enhance resource allocation and promote equitable access to palliative care services. Further research and implementation efforts are warranted to improve access and enhance the delivery of palliative care for lymphoma patients.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal